In the decade since the Affordable Care Act’s (ACA) inception, a critical coverage gap remains in the health insurance landscape.
This gap prevails in the 10 states withholding the ACA Medicaid expansion, affecting 1.5 million uninsured individuals. In this detailed analysis, we investigate who is affected, the potential for expanded coverage, and examine new economic incentives that may prompt a shift towards the adoption of Medicaid expansion in remaining states.
Understanding the Health Insurance Coverage Gap
The ‘Coverage Gap’ is a situation in some states where adults can’t get Medicaid coverage or extra help in the Marketplace because they earn too much. This happened because these states didn’t choose to expand Medicaid under the Affordable Care Act (ACA).
Here’s more on that: The ACA allowed Medicaid to cover adults earning up to 138% of the Federal Poverty Level (FPL), which equals $15,060 per year for a single person in 2024. The federal government even offered to cover most of the cost (90% to be exact) of this expansion.
This change was supposed to make it easier for low-income parents and adults without kids to qualify for Medicaid across all states. But, a 2012 Supreme Court ruling made this expansion optional for states.
So where do we stand now? As of February 2024, 40 states and Washington D.C. have chosen to expand Medicaid.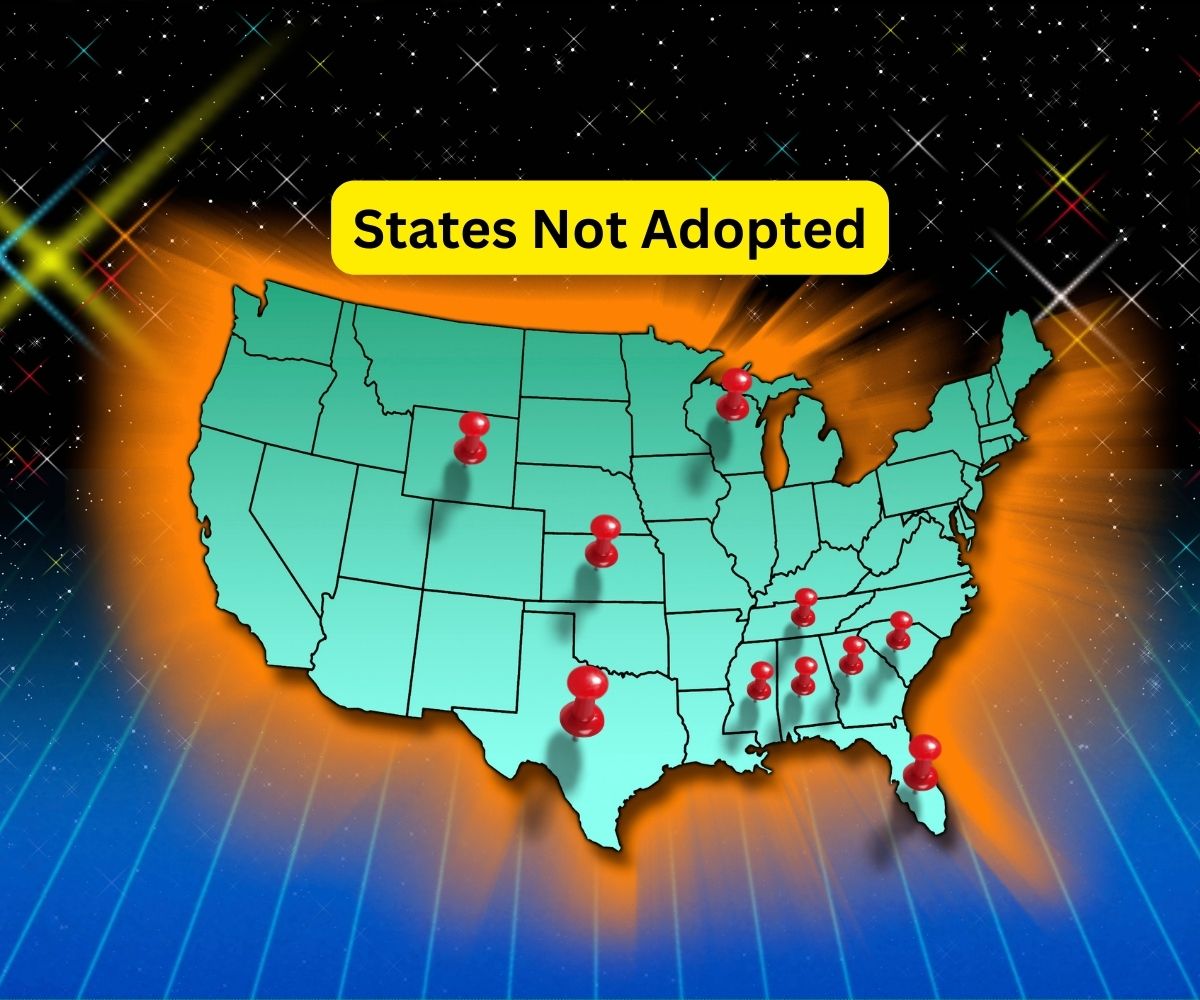
The Southern Disparity
Remarkably, the Southern United States harbors the majority of those in the coverage gap, with states like Texas, Florida, and Georgia accounting for over 70% of the total lacking coverage due to non-expansion. These numbers not only highlight the regional discrepancies in health care access but also underscore the socioeconomic impacts, particularly in the South where larger proportions of the population are low-income and uninsured.
The Fiscal Incentive to Expand
Recent changes in policy, including the introduction of the American Rescue Plan Act (ARPA), now give states a financial reason to expand Medicaid. How so? Well, ARPA promises states that choose to expand Medicaid a temporary boost in the amount they receive from the federal government for their traditional Medicaid programs. This could end up being financially beneficial for these states.
To illustrate this, let’s look at the last two states that expanded Medicaid in 2023 – South Dakota and North Carolina. The numbers show us that these states made substantial financial gains from this move. South Dakota saw fiscal benefits estimated at $60 million, while North Carolina’s benefits reached an impressive $1.2 billion, all within a span of just two years.
The Political Tide Turning?
With the impending unwinding of the Medicaid continuous enrollment provision and rural hospitals in financial peril, some legislative resistance in non-expanding states appears to be waning. The potential financial windfall from the ARPA provisions and the growing awareness of health disparities may catalyze Medicaid expansion in the holdout states. South Dakota and North Carolina’s recent expansion adoption could serve as exemplars of financial and health coverage benefits reaped from such policy changes.
Conclusion
The convergence of enhanced federal funding opportunities, the fiscal strain on health systems, and the spotlight on disparities may indeed be shifting the Medicaid expansion landscape. While it remains unclear how many of the remaining states will pivot to adopt the expansion, the incentives to do so have never been clearer. Should more states join the ranks of expansion adopters, the long-standing coverage gap affecting millions could rapidly shrink, leading towards a more equitable health insurance system across the nation.

